Body Mass Index (BMI)
Body Mass Index (BMI) is a commonly known formula used to estimate body fat percentage as a function of the BMI indexing system. The use of BMI is now ubiquitous in America as seen by its use in nearly all health care related metrics to include physicals and health insurance. The term Body Mass Index is used in numerous studies such as Ode, J. J., (2007). “Body Mass Index as a Predictor of Percent Fat in College Athletes and Nonathletes.” and Tomiyama, A. J., (2016), “Misclassification of cardiometabolic health when using body mass index categories in NHANES 2005–2012.”
The two measurements used in the BMI calculation are HEIGHT and WEIGHT. When entering these two variables for the individual pictured below, his BMI is 38 which is classified as OBESE.
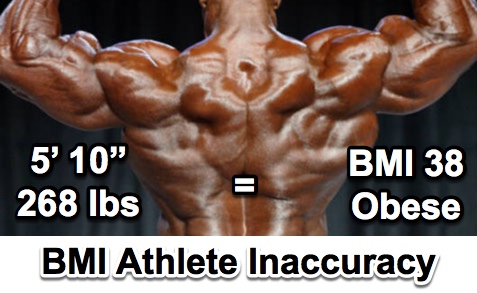
Some studies suggest that BMI may be highly inaccurate for certain groups (Tomiyama, A. J., et al., 2016), but especially very athletic individuals (Ode, J. J., et al., 2007). Since a select volume of muscle is much more dense than the same volume of fat, using weight and height only in the BMI calculation cannot account accurately for this discrepancy (Visit our BODY DENSITY page).
In one study, Ode, J. J., (2007), attempted “1) to describe the relationship between BMI and % fat, and 2) to determine the accuracy of BMI as a measure of % fat in college athletes and nonathletes.” The researchers in this study deemed it “critical” to understand this relationship since BMI is being used as a default to label athletes and the young as obese (Ode, J. J., et al., 2007). The researchers proposed that different “cutpoints” with regard to the obesity designation in BMI for athletes and the young should be considered to account for the variances in muscle mass.
In a study by Tomiyama, A. J.,(2016), data from over 40,000 “individuals aged 18+ in the nationally representative 2005–2012 National Health and Nutrition Examination Survey” was analyzed in order to determine the accuracy of BMI as an indicator of health. Their “results clearly indicate that health policies such as those proposed by the Equal Employment Opportunity Commission (EEOC) should not rely on BMI. Not only are such policies discriminatory, but they run the risk of overlooking more effective approaches.” (Tomiyama, A. J., et al., 2016). The researchers indicated that using blood markers would be a much more effective and accurate measure of health, but acknowledged that “…if lab markers are absolutely unobtainable, potential solutions are to instead use markers that researchers argue are a more accurate marker of health than BMI, such as physical activity and cardiorespiratory fitness, waist circumference or body fat percentage, or their combination.”
BMI and Health Insurance
Potential BMI inaccuracy would not be an issue worth addressing in such a definitive and comprehensive manner as is being put forth here, as well as in other research papers, if it were only referenced as a minor supplemental metric within other major physical examination data taken of individuals. This issue potentially affects individuals in numerous areas which may have serious repercussions.  Health plans use BMI to make determinations as to the type of health assistance programs one may need to become healthier; an inaccurate BMI leads to inaccurate health ratings and assigned programs to make one “healthier”. An inaccurate BMI can create real, financial issues when it is used incorrectly by health insurers to rate the premiums one receives in a healthcare plan, possibly creating a discrimination where there should be none.
Health plans use BMI to make determinations as to the type of health assistance programs one may need to become healthier; an inaccurate BMI leads to inaccurate health ratings and assigned programs to make one “healthier”. An inaccurate BMI can create real, financial issues when it is used incorrectly by health insurers to rate the premiums one receives in a healthcare plan, possibly creating a discrimination where there should be none.
This is explicitly observed in an Associated Press article presented by an NBCnews.com. article entitled, “Shrink Your BMI — And Your Insurance Bill”. This article discusses an example of how BMI is being used to determine a billing structure for employee’s healthcare costs. In the article, “Dr. Rob Kinney, vice president and medical director of The Phoenix, said BMI is a good measure of longevity, which is the first consideration for a life insurance company.” When applying the research results from a study as recent as March, 2016 by Tomiyama, A. J.,(2016), “…found that close to half of Americans who are considered “overweight” by virtue of their BMIs (47.4 percent, or 34.4 million people) are healthy, as are 19.8 million who are considered ‘obese.’” This indicates a percentage that closely resembles that of flipping a coin to assign an indicator of one’s health. This in turn may indicate that the many research papers using inaccurate BMI numbers in their analyses, describing conclusions of health prognostication based on this inaccurate number, are thus rendering inaccurate conclusions by necessity. Athletes at an organization such as the one listed in the NBC article are at a distinct disadvantage when purchasing life insurance.
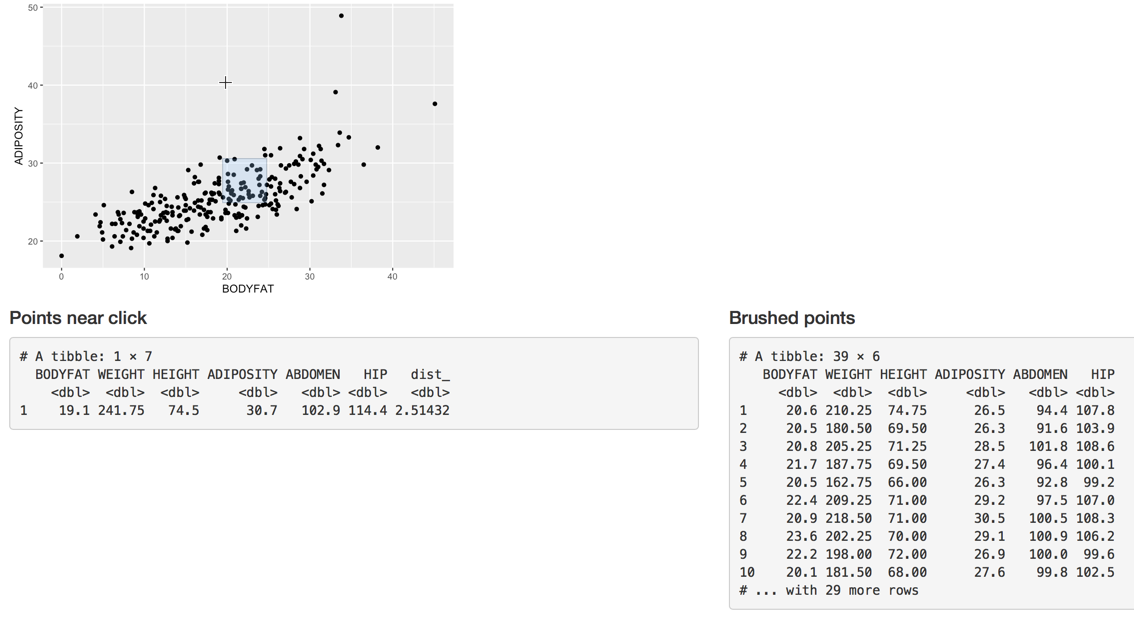 Adiposity(BMI) - Body Fat% Interactive Plot
Adiposity(BMI) - Body Fat% Interactive Plot
The graph above provides a look at the relationship, or correlation, between body fat percentage (BODYFAT on the horizontal axis) and BMI (ADIPOSITY on the vertical axis). When there is a high correlation between the two variables, the points will generally be very close together along a line that is either straight or curved. As this graph shows, there is some indication of a grouping along a line angled upward to the right. The grouping of the data points however is rather loose, suggesting a weaker association than if they were closer together. Clicking the link below the title will open an interactive app allowing you to select points or groups of points (brushing or creating a selector box) in order to view additional information tied to the points (individuals who were measured for this data).
Other formulas have been developed to address some of the issues associated with the Body Mass Index.